Muscle relaxers are used in addition to rest, physical therapy, and other measures to relieve discomfort. They are typically prescribed for short-term use to treat acute, painful musculoskeletal conditions. Muscle relaxers are occasionally prescribed for chronic pain (pain lasting longer than 3 months).
Muscle relaxers are not a class of drugs—meaning they do not all have the same chemical structure or work the same way in the brain. Rather, the term muscle relaxer is used to describe a group of drugs that act as central nervous system depressants and have sedative and musculoskeletal relaxant properties.
Muscle relaxers may be prescribed to treat back pain:
- Early in the course of back pain, on a short-term basis, to relieve pain associated with muscle spasms
- When back pain causes insomnia (for their sedative effect)
Muscle relaxers are also prescribed for other conditions such as fibromyalgia, multiple sclerosis, and seizure disorders.
There are several types of muscle relaxer medications commonly used to treat back pain.
Common Muscle Relaxants
Muscle relaxers are usually prescribed to treat back pain in conjunction with rest and physical therapy. Common muscle relaxants include:
- Baclofen. Muscle tightness and muscle spasms, including those related to spine injuries, may be eased with baclofen. The medication may be helpful in treating multiple sclerosis and stabbing nerve pain. It is available as a tablet and can be taken by children as young as 12 years old. Some common side effects could include nausea and vomiting, confusion, drowsiness, headache, or muscle weakness. Baclofen is rated C in the FDA’s A through X pregnancy safety ranking for medications, with A being the safest. The C category means that the medication should only be used if the benefits outweigh the risks.
- Benzodiazepines. In addition to treating anxiety, alcohol withdrawal, and seizure disorders, such as epilepsy, benzodiazepines can also treat muscle spasms and skeletal pain. Benzodiazepines, such as diazepam (Valium), lorazepam (Ativan), and temazepam (Restoril), are typically only intended for short-term use. This limitation is due to their habit-forming potential and because they alter sleep cycles, leading to sleep difficulties once the drug is stopped. Benzodiazepines are sold as tablets, liquid, injections, and rectal gels. People who have myasthenia gravis, severe liver disease, serious breathing troubles, or some forms of glaucoma, should avoid taking diazepam. All benzodiazepines are rated D by the FDA for safety during pregnancy and are not recommended for women who are pregnant.
- Carisoprodol (Soma). Carisoprodol relaxes muscles and eases pain and stiffness caused by acute bone and muscle problems, often caused by an injury. It is taken by mouth in tablet form and is also available in combination with aspirin or aspirin and codeine. Carisoprodol can be habit-forming, particularly if used in conjunction with alcohol or other drugs that have a sedative effect, including opioids (such as codeine). Common side effects include drowsiness, dizziness, and headache. People with a history of blood disorders, kidney or liver disease, and seizures may need to avoid Carisoprodol. It is rated C in the FDA’s pregnancy safety ranking for medications.
- Chlorzoxazone (Lorzone). Chlorzoxazone is used for the relief of discomfort from acute, painful, musculoskeletal conditions. Chlorzoxazone is available as a tablet. Common side effects include drowsiness, dizziness, and nausea. Chlorzoxazone is not recommended for people with liver disease. It has not been rated by the FDA for safety during pregnancy.
- Cyclobenzaprine (Amrix, Fexmid, FlexePax Kit, FusePaq Tabradol). Cyclobenzaprine eases stiffness and pain from muscle cramps, also called muscle spasms. It is available as a tablet and extended-release capsule. Cyclobenzaprine itself is not intended for long-term use (more than 2 to 3 weeks).
 Common side effects include blurred vision, dizziness or drowsiness, and dry mouth. It is not advised for those with an overactive thyroid, heart problems, or liver disease. Cyclobenzaprine is rated B by the FDA for safety during pregnancy, making it the safest muscle relaxant to use while pregnant.
Common side effects include blurred vision, dizziness or drowsiness, and dry mouth. It is not advised for those with an overactive thyroid, heart problems, or liver disease. Cyclobenzaprine is rated B by the FDA for safety during pregnancy, making it the safest muscle relaxant to use while pregnant. - Dantrolene (Dantrium). Dantrolene helps control chronic spasticity related to spinal injuries. It is also used for conditions such as stroke, multiple sclerosis, and cerebral palsy. Dantrolene is taken as a capsule or intravenous powder for injection. Drowsiness and sensitivity to light are common side effects. It can cause severe liver problems, and should not be taken by people with active liver disease. The FDA has given dantrolene a C rating for safety in pregnancy.
- Metaxalone (Skelaxin, Metaxall, and Metaxall CP, Lorvatus PharmaPak). Metaxalone targets pain and muscle spasms from sprains, strains, and muscle injuries. It is available as a tablet or injection. Common side effects include drowsiness, dizziness, nausea, and vomiting. Metaxalone is generally not recommended for people with a known tendency to become anemic, and who have kidney or liver disease. Metaxalone may affect blood sugar tests for people with diabetes. The FDA has not rated metaxalone for safety during pregnancy.
- Methocarbamol (Robaxin, Robaxin-750). Methocarbamol eases acute muscle and bone pain. It can be taken as a tablet or by injection.
 Common side effects include dizziness, headache, nausea, flushing, and blurred vision. Methocarbamol is generally not recommended to people with renal disease or failure, or a history of allergic reaction to the medication. The FDA has given methocarbamol a C rating for safety during pregnancy.
Common side effects include dizziness, headache, nausea, flushing, and blurred vision. Methocarbamol is generally not recommended to people with renal disease or failure, or a history of allergic reaction to the medication. The FDA has given methocarbamol a C rating for safety during pregnancy. - Orphenadrine. Orphenadrine is a medication used to relieve pain and stiffness caused by muscle injuries. It is available as an extended-release tablet. Common side effects include dry mouth, lightheadedness, difficult urination, heartburn, nausea and vomiting. It is generally not recommended to people with previous sensitivities to the ingredients, myasthenia gravis, those with glaucoma or certain types of ulcers. The FDA has given orphenadrine a C rating for safety during pregnancy.
- Tizanidine (Comfort Pac with Tizanidine, Zanaflex). Tizanidine is used to treat muscle spasms caused by spinal cord injuries and other conditions such as multiple sclerosis. Tizanidine is available in tablet and capsule form and absorbs differently depending on whether it is taken on an empty stomach or with food.
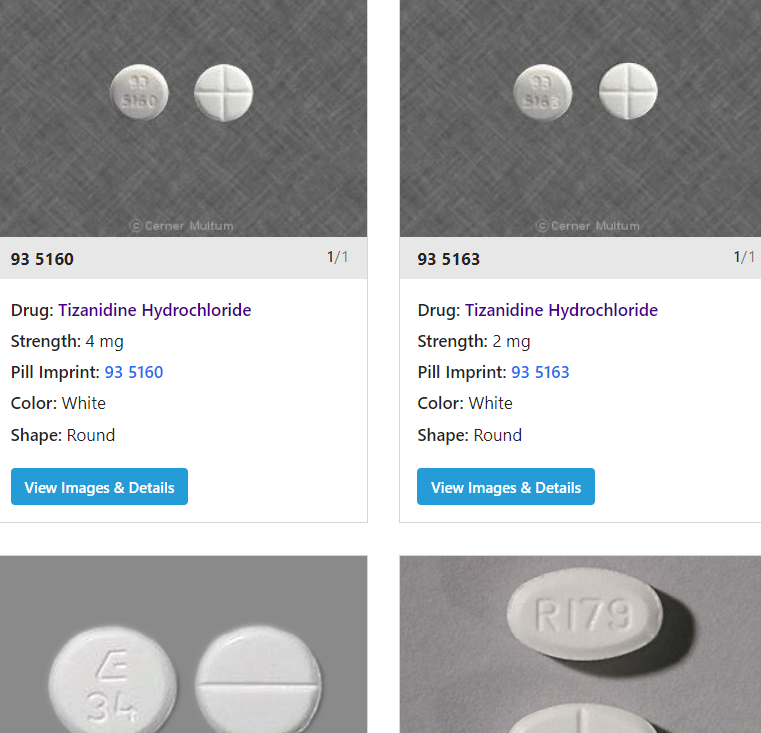
- Common side effects include dry mouth, dizziness, constipation and tiredness. It should not be used by people taking fluvoxamine or ciprofloxacin or those who have liver disease. Tizanidine is rated in the C category for safety during pregnancy.
Sometimes the first muscle relaxers a doctor prescribes does not work as well as expected. It may be necessary to try an alternative if the initial prescription is not effective. Many drugs interact with muscle relaxers and a person should keep their health care provider informed of all prescription and non-prescription medications he or she is taking.
There is very little research regarding which muscle relaxers are most effective, so the choice of which medication—or whether to use one at all—is based on factors such as a person’s reaction to the medication and personal preferences, potential for abuse, possible drug interactions, and adverse side effects.
Medication is just one part of pain relief. These medications are intended to be one element, usually on a short-term basis, of an overall recovery strategy that includes rest, stretching, physical therapy, and other exercise.
About Soma ( Carisoprodol )
Carisoprodol, sold under the brand name Soma among others, is a medication used for musculoskeletal pain. Use is only approved for up to three weeks. Effects generally begin within half an hour and last for up to six hours. It is taken by mouth.
Common side effects include headache, dizziness, and sleepiness. Serious side effect may include addiction, allergic reactions, and seizures. In people with a sulfa allergy certain formulations may result in problems. Safety during pregnancy and breastfeeding is not clear. How it works is not clear. Some of its effects are believed to occur following being converted into meprobamate.
Carisoprodol is meant to be used along with rest, physical therapy and other measure to relax muscles after strains, sprains and muscle injuries. It comes in tablet format and is taken by the mouth three times a day and before bed.
Carisoprodol was approved for medical use in the United States in 1959. Its approval in Europe was withdrawn in 2008. It is available as a generic medication. In the United States the wholesale cost is less than US$0.10 per dose. In 2017, it was the 255th most commonly prescribed medication in the United States, with more than one million prescriptions. In the United States, it is a Schedule IV controlled substance.
Soma ( Carisoprodol ) is a controlled prescription and we can not sell it online. It is also illegal for you to buy Soma ( Carisoprodol ) online.
Side Effects Associated with Muscle Relaxers
Side effects of muscle relaxers include:
- Sleepiness or grogginess
- Fatigue
- Dry mouth
- Constipation
- Nausea
More serious side effects include:
- Light-headedness or fainting
- Blurred vision
- Confusion
- Urinary retention
Any serious side effects should be reported to a doctor immediately.
Warnings for prescription muscle relaxants
Muscle relaxants such as carisoprodol and diazepam can be habit forming. Be sure to take your medication exactly as prescribed by your doctor.
Muscle relaxants can also cause withdrawal symptoms, such as seizures or hallucinations (sensing things that aren’t real). Do not suddenly stop taking your medication, especially if you’ve been taking it for a long time.
Also, muscle relaxants depress your central nervous system (CNS), making it hard to pay attention or stay awake. While taking a muscle relaxant, avoid activities that require mental alertness or coordination, such as driving or using heavy machinery.
You should not take muscle relaxants with:
- alcohol
- CNS depressant drugs, such as opioids or psychotropics
- sleeping medications
- herbal supplements such as St. John’s wort
Talk to your doctor about how you can safely use muscle relaxants if you:
- are older than 65 years
- have a mental health problem or brain disorder
- have liver problems
Off-label medications for spasticity
Doctors can use certain medications to treat spasticity even when the drugs are not approved for that purpose by the U.S. Food and Drug Association (FDA). This is called off-label drug use. The following drugs are not actually muscle relaxants, but they can still help relieve symptoms of spasticity.
Benzodiazepines
Benzodiazepines are sedatives that can help relax muscles. They work by increasing the effects of certain neurotransmitters, which are chemicals that relay messages between your brain cells.
Examples of benzodiazepines include:
- clonazepam (Klonopin)
- lorazepam (Ativan)
- alprazolam (Xanax)
Side effects of benzodiazepines can include drowsiness and problems with balance and memory. These drugs can also be habit forming.
Clonidine
Clonidine (Kapvay) is thought to work by preventing your nerves from sending pain signals to your brain or by causing a sedative effect.
Clonidine should not be used with other muscle relaxants. Taking it with similar drugs increases your risk of side effects. For instance, taking clonidine with tizanidine can cause very low blood pressure.
Clonidine is available in brand-name and generic versions.
Gabapentin
Gabapentin (Neurontin) is an anticonvulsant drug typically used to relieve seizures. It’s not fully known how gabapentin works to relieve muscle spasticity. Gabapentin is available in brand-name and generic versions.
Over-the-counter options for muscle spasms
OTC treatment is recommended as first-line therapy for muscle spasms caused by conditions such as acute lower back pain or tension headache. This means you should try OTC treatments before prescription medications.
OTC treatment options include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, or a combination of both. Your doctor or pharmacist can help you choose an OTC treatment.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
NSAIDs work by blocking your body from making certain substances that cause inflammation and pain. NSAIDs are available in generic and brand-name versions. They’re typically sold over the counter. Stronger versions are available by prescription.
NSAIDs come as oral tablets, capsules, or suspensions. They also come as chewable tablets for children. Side effects of these drugs can include upset stomach and dizziness.
Examples of NSAIDs include:
- ibuprofen (Advil, Motrin)
- naproxen (Aleve)

Acetaminophen
Acetaminophen (Tylenol) is thought to work by blocking your body from making certain substances that cause pain. Acetaminophen is available in generic and brand-name versions. It comes as immediate-release and extended release oral tablets and capsules, orally disintegrating tablets, chewable tablets, and oral solutions.
The more common side effects of acetaminophen can include nausea and upset stomach.
Can cannabis be used to treat muscle spasticity or spasm?
Yes, in some cases.
Cannabis, more commonly known as marijuana, is legal in certain states for medicinal uses. Muscle spasm is one of the health conditions that cannabis is used to treat. It helps relieve muscle spasms by reducing pain and inflammation.
Cannabis has also been used to treat muscle spasticity due to multiple sclerosis (MS). In many research trialsTrusted Source, cannabis has been shown to be effective alone and in combination with other treatments for reducing muscle spasticity symptoms. However, there’s limited information available on the use of cannabis for muscle spasticity that’s not associated with MS.
If you’re being treated for MS and still have muscle spasms or spasticity, adding cannabis may help. Talk to your doctor about whether it’s a good option for you.
You should keep certain factors in mind. The more common side effects of cannabis include dizziness, vomiting, urinary tract infections, and a relapse of MS. Also, limited information is available about drug interactions and other usage warnings.
Risks Associated with Muscle Relaxers
Muscle relaxers are a group of drugs that have a sedative effect on the body. They work through the brain, rather than directly on the muscles. Muscle relaxants are generally used for a few days and up to 3 weeks, but are sometimes prescribed for chronic back pain or neck pain.
To minimize risk, the doctor should be informed of any history of seizures, liver disease, and any other medical conditions or concerns. Women should inform their doctors if they are pregnant, plan to become pregnant, or are breast-feeding.
- Sleepiness. Because muscle relaxers are total body relaxants, they typically induce grogginess or sleepiness. As a result, it is not safe to drive or make important decisions while taking muscle relaxers. Muscle relaxers are often suggested for evening use due to their sedative effect.
- Interactions with alcohol. Drinking alcohol can be especially dangerous when taking muscle relaxers. The sedative effect of the medication is intensified with alcohol use, and combining the two can be fatal.See Alcohol Avoidance
- Allergic reactions. No medication should be taken if the person has had an allergic reaction to it in the past, even if the reaction seemed mild. Symptoms of an allergic reaction include swelling in the throat or extremities, trouble breathing, hives, and chest tightness.
- Potential for abuse. Muscle relaxers have a risk of misuse and abuse. Some muscle relaxers, such as cyclobenzaprine, can be habit-forming on their own. Others may be taken in conjunction with other drugs, such as opioids, to create a high, and are therefore more likely to be abused.See Opioids for Back Pain: Potential for Abuse, Assessment Tools, and Addiction Treatment
- Tapering off. Stopping a muscle relaxer abruptly can be harmful. Instead, the doctor will prescribe a gradual reduction in dosage.
Concern About Overuse of Muscle Relaxants
The use of muscle relaxers is controversial in the medical community. The growing use of these medications has drawn concern about overuse, adverse side effects, and limited evidence of their effectiveness—especially when used on an ongoing basis for a chronic condition.
Research is mixed on muscle relaxers. A number of research studies and analyses have found muscle relaxants to be more helpful than a placebo in easing symptoms of nonspecific acute low back pain in the short term.1,2 Other research, however, found that people visiting an emergency room for back pain received no additional benefit from taking muscle relaxers.3
What is the best muscle relaxer?
It’s difficult to declare one muscle relaxant better than all others because each type has its own advantages and uses. In general, pain relief treatments fall into one of three categories: over-the-counter (OTC), prescription, and natural. Determining the best muscle relaxer depends entirely on your specific condition and pain level. When in doubt, consult your healthcare provider.
Over-the-counter remedies: OTC pain relievers are often the first line of defense against pain, inflammation, and tension. They can work wonders for milder conditions like neck and lower back pain. Typically, your doctor might start you out on an OTC medication, and if that doesn’t provide the relief you need, he or she may write a prescription for something higher-grade.
Prescription drugs: For more chronic pain and conditions where OTC medications just won’t cut it, your doctor may prescribe something stronger. Because of their more serious side effects, prescription muscle relaxers are designed for short-term use, after which your doctor will transition to other drugs or treatments.
Natural remedies: For minor soreness and stress-related symptoms, the only treatment you need might be drawn straight from nature. Before rushing off to the doctor for an examination and potential prescription, you might be able to administer an effective plant-based therapy right from home.
What is the best over-the-counter (OTC) medicine for muscle pain?
These are the medications that you can find while perusing the aisles at your local pharmacy or convenience store. Most of them are household names, and it’s not uncommon to keep them on hand, stashed in a medicine cabinet, just in case. Even though OTC medications are easy to obtain, they’ll do the job for many aches and pains, and doctors often recommend them prior to prescribing stronger treatment options.
“OTC NSAIDS, like ibuprofen and naproxen, are a good first line agent to decrease inflammation surrounding an injury,” recommends Joanna Lewis, Pharm.D., creator of The Pharmacist’s Guide. They might not have the same potency of high-grade muscle relaxants, but they’re still effective and have very few side effects. If you roll your ankle at the gym or wake up with back pain, try one of these before asking your doctor for a prescription.
- Advil (ibuprofen): This is a staple of parents, doctors, and athletes alike. Ibuprofen is one of the most widely used nonsteroidal anti-inflammatory drugs (NSAIDs) available. As such, Advil doesn’t just remedy pain, but also inflammation as well. It’s highly versatile. Use it to treat low back pain, osteoarthritis, menstrual cramps, fever, headaches, migraines, sprains, and other minor injuries. Low doses are available over the counter, but a doctor can prescribe higher doses as well.
- Motrin IB (ibuprofen): Don’t be fooled by the different brand name. Motrin IB and Advil are the same drug. Therefore, they shouldn’t be taken together, as it could increase the risk of overdose.
- Aleve (naproxen): Another medicine cabinet staple, naproxen is similar to ibuprofen in many ways. It’s also an NSAID, so it works by reducing inflammation. It’s useful in treating muscle pain, headaches, migraines, osteoarthritis, fever, cramps, and minor injuries. The main difference between naproxen and ibuprofen is their dosing. You can take naproxen every eight to 12 hours and ibuprofen every four to six, so Aleve is slightly longer-lasting.
- Aspirin: One more NSAID for you. Aspirin treats many of the same conditions, relieving pain and reducing inflammation. However, daily doses of aspirin have been proven effective at reducing the risk of blood clots, strokes, and heart attacks in some people. Ask your doctor before using for clot prevention. If you’re a candidate, you will likely take a “baby” aspirin, or 81 mg, coated tablet daily. Common brand names include Bayer or Ecotrin.
- Tylenol (acetaminophen): Unlike NSAIDs, acetaminophen focuses solely on treating pain—not inflammation. It’s used for muscle aches, headaches, migraines, back and neck pain, fevers, etc. However, if swelling and inflammation is the underlying cause of your pain, acetaminophen will not be nearly as effective as NSAIDs like those listed above. Acetaminophen’s wide range of uses and relatively few side effects make it the most popular OTC pain reliever worldwide.
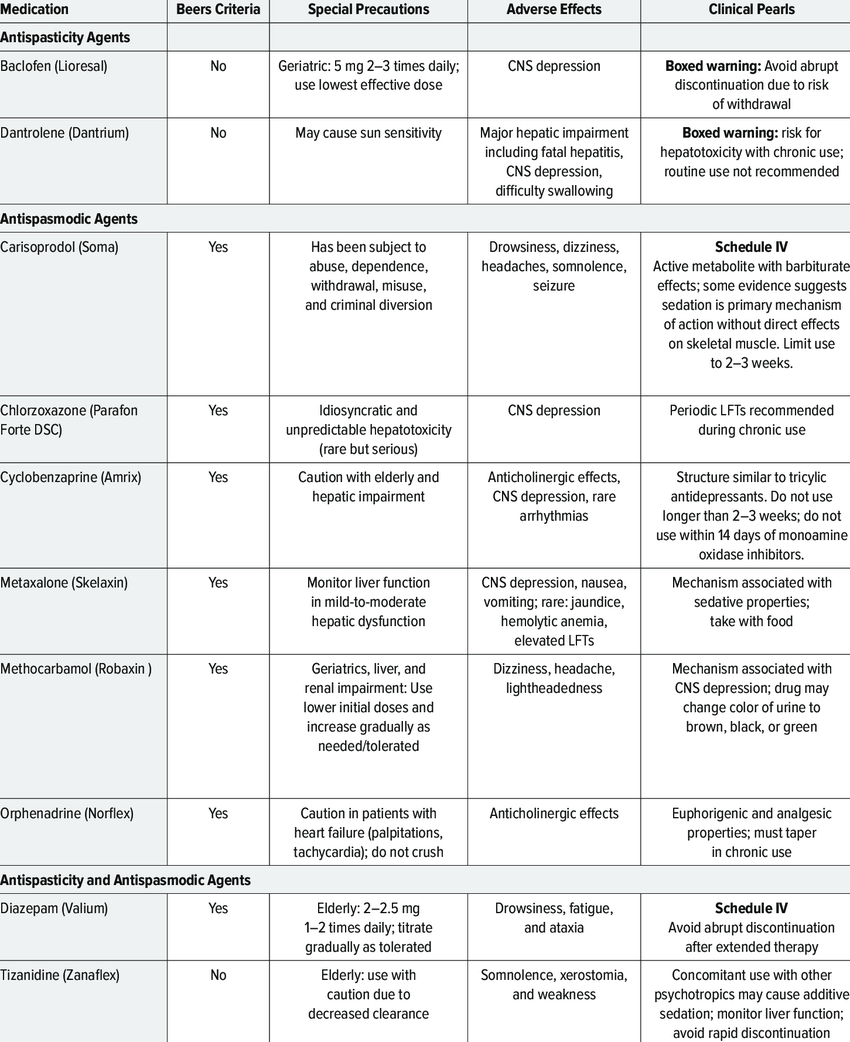
Antispasmodic drugs are better for relieving muscle pain due to uncontrolled muscle contractions.
The following are muscle relaxants classified as antispasticity drugs:
- baclofen (Lioresal)
- dantrolene (Dantrium)
The following muscle relaxants are considered antispasmodic drugs:
- carisoprodol (Soma)
- chlorzoxazone (Parafon Forte)
- cyclobenzaprine (Flexeril, Amrix)
- methocarbamol (Robaxin)
- orphenadrine (Norflex)
The following medications are classified as both antispasticity and antispasmodic medications:
- diazepam (Valium)
- tizanidine (Zanaflex)



found this once cant find again,,muscle lwg oain relief
Off-label Medications for Spasticity
Over-the-counter Options for Muscle Spasms
Antispasmodics: Centrally Acting Skeletal Muscle Relaxers
Antispastics
Understanding Spasticity Versus Spasm
Muscle relaxants treat two conditions: spasticity and spasm. Spasticity is marked by long-term muscle contraction caused by a brain or spinal cord injury. Spasms, on the other hand, are localized and occur because of a musculoskeletal issue.
Prescription muscle relaxants fall into 2 groups: antispastics and antispasmodics.
While some antispasmodics may treat spasticity in addition to spasms, antispastics should not be used to treat spasms.
Antispasmodics: Centrally Acting Skeletal Muscle Relaxers
Antispastics
Common Muscle Relaxants